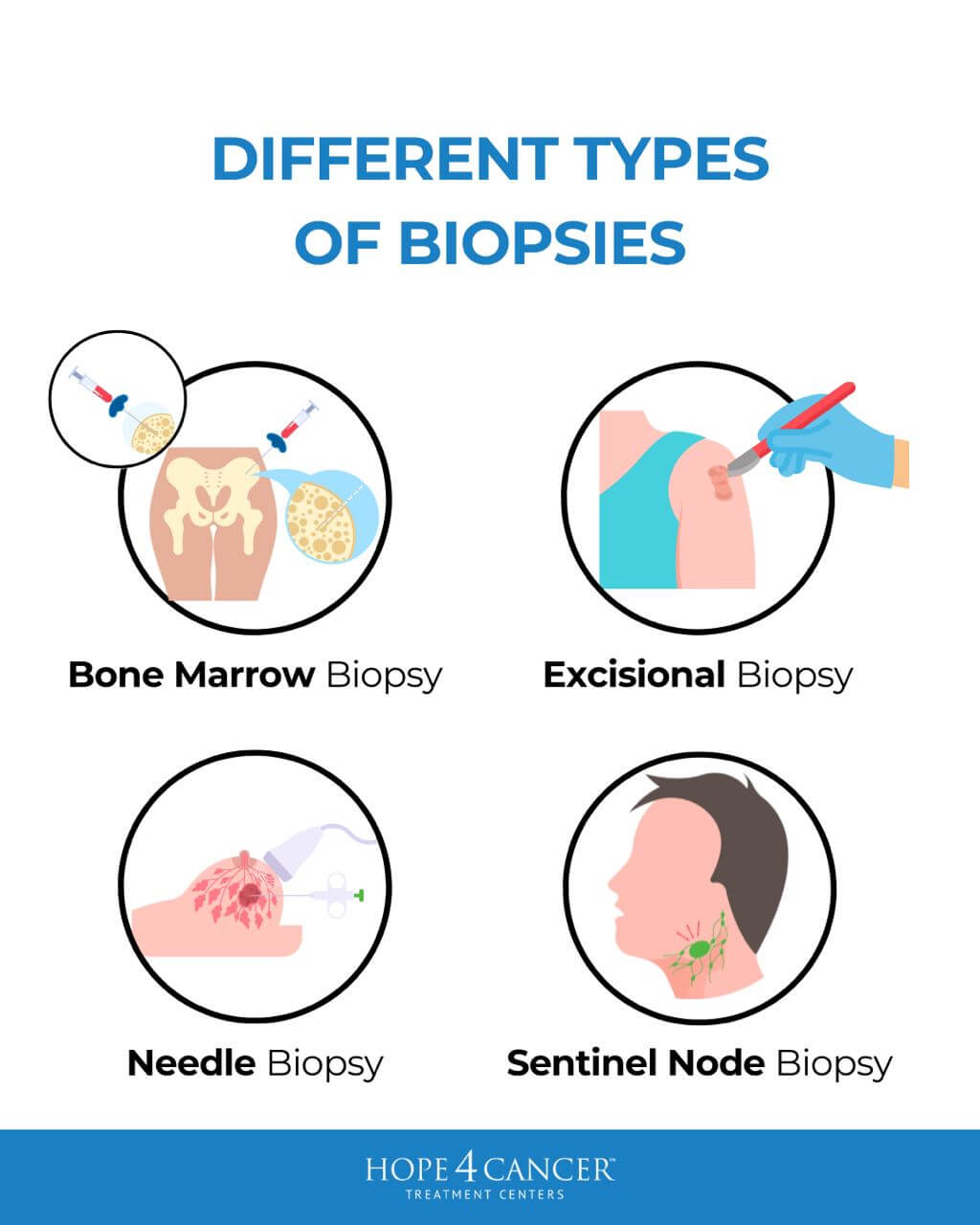
Biopsies are a crucial diagnostic tool in cancer diagnosis and management, involving the removal of cells or tissues for examination to determine the presence or extent of a disease. Various types of biopsies, such as bone marrow, skin, endoscopic, and surgical biopsies, are used depending on the location and nature of the suspected malignancy. Particularly common in cancer diagnostics are needle biopsies, which use a needle to extract tissue samples from a tumor.
Biopsies are considered the gold standard for accurately diagnosing and staging cancer. However, while these procedures can be valuable for their diagnostic accuracy, they are not without risks. In this medical opinion article, we will primarily focus on needle biopsies and the documented risk of needle tract seeding—a process where cancer cells are dislodged and spread along the path of the biopsy needle.
As advancements in needle biopsy techniques and cancer treatments have evolved, so too has our understanding of the risks associated with these procedures. Along with the improvement in the associated technologies, the precision and frequency of biopsies have increased, bringing the potential for seeding into sharper focus. So, what does the current research indicate about this risk? Are biopsies a cause for concern, and what does the future hold for minimizing complications while maximizing diagnostic benefits?
Introduction to Needle Biopsies
Before discussing the specific risks of needle biopsies, it’s important to understand the various types commonly used in cancer diagnosis. Each method comes with its own techniques, advantages and disadvantages, and associated risks of seeding:
- Fine Needle Aspiration (FNA) collects cells with a thin needle and is generally less invasive, minimizing tissue disruption and potentially reducing the risk of seeding. However, because it only provides small samples, it may not provide enough information about the nature of the tumor.
- Core Needle Biopsy (CNB) uses a larger needle to remove a tissue core. This preserves the tissue’s architecture but involves greater manipulation of the tumor, possibly increasing the risk of seeding.
- Vacuum-Assisted Biopsy (VAB) utilizes suction to gather multiple samples through one needle insertion, effectively reducing the total number of penetrations. This potentially lowers the risk of seeding compared to CNBs—however, it is a more invasive procedure.
- Image-Guided Biopsies utilize ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) to accurately guide the biopsy needle to the target area. This precision reduces the need for multiple needle insertions, reducing the risk of seeding.
Needle Tract Seeding: The Research and Risks
While the above needle biopsy methods have been refined over the years to improve precision, the risk of needle tract seeding still presents a concern. Conventional medicine often downplays the likelihood of seeding, suggesting it is a minimal or nonexistent risk. Even though small, the risk is real, as evidenced by numerous studies that have documented and analyzed this phenomenon. For example, one study of 4500 participants with breast cancer found that seeding was confirmed in 3% of patients who received a core needle biopsy (CNB) or vacuum-assisted biopsy (VAB) (1). Other studies have shown that 22% to 50% of biopsies using 14–18G needles (usually used for CNBs) resulted in needle tract seeding, even though the reporting of local recurrence is rare (2).
Of note, many reported instances of seeding involve breast cancer, likely due to the high frequency of biopsies performed on breast tumors. The pliable and accessible nature of breast tissue allows for easier needle insertion and typically yields high-quality samples, facilitating clear and accurate diagnoses. This very effectiveness and frequent usage, however, also contribute to a higher number of reported cases of seeding. Yet, it is important to note that seeding is not exclusive to breast cancer; instances have been observed in various other types of cancer as well, indicating that this is a broader issue within oncology that requires attention.
The reason seeding is particularly concerning is that it can potentially lead to the cancer spreading. There is always the potential that the dislodged cancer cells can begin to grow anew at the site of the biopsy or along the needle path. This seeding can create new cancer cell clusters that could grow into recurrent tumors after treatment. Numerous case studies clearly demonstrate this phenomenon (2-4). For instance, a 2021 study documented a patient with invasive mucinous carcinoma of the breast who had malignant cell seeding within the biopsy tract confirmed via MRI (5). Another study reported three patients with breast cancer recurrence at their biopsy sites, suggesting that tumor cells can indeed seed the needle tract and lead to significant recurrences post-surgery (6). These examples underscore that seeding is a well-documented risk.
As a side note, new research shows that tumors harbor a great deal of stress within them (known as “solid stress”), a feature that is considered to be one of their four physical traits (7, 8). Cutting or poking tumors relieves that stress, and causes tumors to expand, potentially allowing cancer cells to disseminate. While data on the contribution of solid stress to tumor growth and metastasis is limited, there is a theoretical possibility of this being a risk factor of biopsies.
Does Seeding Necessarily Lead to Recurrence or Decreased Survival?
It’s essential to recognize that many patients experience needle tract seeding without ever developing further complications. In fact, a significant portion of those with documented seeding do not go on to have cancer recurrence. This may be partly explained by the nature of the seeded cells themselves—many are likely unviable and are effectively eliminated by the body’s immune system. However, as the evidence suggests, this elimination is not guaranteed in every case. Despite the immune system’s capability to address these stray cells, the incidence of recurrence in some patients highlights that this defense is not foolproof and that seeding can sometimes lead to serious outcomes.
Another complicating factor is that when a cancer patient develops metastasis, pinpointing the exact cause can be exceedingly difficult or even impossible. Determining whether metastasis arose naturally from the progression of the disease or whether it could be attributed to seeding during a biopsy is often unclear due to the complex nature of cancer and its ability to spread through various mechanisms. We simply don’t have enough definitive data to trace every instance of metastasis back to its cause.
Perhaps the most important consideration of all is the comparison of survival rates between patients who have undergone biopsies and those who have not. Current research does not indicate that biopsies decrease survival rates, even in the case of seeding and recurrence. Indeed, studies that have compared groups of patients who experienced seeding post-biopsy with those who did not have often found that seeding does not necessarily result in worse outcomes (1, 9). This suggests that while the phenomenon of seeding is a concern, its impact on long-term survival might be less dire than assumed. However, more comprehensive research is needed to fully understand the implications and ensure that medical practices continue to improve, adapt, and avoid unnecessary procedures that may expose patients to undue risks.
Making Informed Choices About Biopsies
Making medical decisions often involves weighing potential risks and benefits, and no decision is entirely without risk. Each person’s situation is unique, influenced by their specific type of cancer, personal experiences, and their tolerance for risk. When considering whether a biopsy is appropriate for your situation, it’s crucial to have an open and thorough discussion with a trusted healthcare provider. Key questions to ask include:
- Is the biopsy necessary for accurate diagnosis, or are there alternative methods that could provide sufficient information?
- What are the potential benefits of obtaining a precise diagnosis with a biopsy compared to the risks involved?
- Is it possible to perform a surgical or excisional biopsy, where the tumor is analyzed after the intact mass is surgically removed, leaving behind clean margins? Doing so could eliminate the risk of seeding, as the microscopic analysis would be conducted by sampling the removed tissue.
- Are there less invasive options available for cancer diagnosis? If so, what types of cancer are they suitable for, and what can they tell us?
The Impact of Biopsies on Quality of Life and Overtreatment
Aside from seeding, biopsies are invasive procedures that can impact a patient’s quality of life. Side effects and complications can include pain, bleeding, infections, or psychological distress. These challenges highlight the importance of considering all potential risks and carefully evaluating the necessity of a biopsy in the broader context of a patient’s overall health and quality of life.
While the direct impacts of biopsies on patient well-being can be significant, the decisions following these diagnostic tests can also lead to something called overtreatment. Overtreatment occurs when a detected cancer is treated more aggressively than may be necessary, especially in cases where the cancer is slow-growing and not immediately life-threatening.
In prostate cancer, for instance, aggressive treatment following a positive biopsy result can lead to significant side effects, such as urinary incontinence and sexual dysfunction, without substantially improving survival outcomes. As explored in an earlier blog post, early detection of prostate cancer does not always correlate with increased survival rates. This is due to the often slow progression of the disease, where many men may live with the condition without it becoming fatal.
Biopsy decisions should, therefore, be made with a comprehensive understanding of both the potential benefits and the risks. Patients must consider their personal health circumstances, the type of cancer suspected, and the likelihood of being able to tailor their treatment plan based on the results obtained from the biopsy. Discussions with healthcare providers should focus on these considerations, aiming to tailor the diagnostic process to the individual’s specific needs while avoiding unnecessary procedures. This balanced approach is essential to ensure that the benefits of biopsies in diagnosing and managing cancer are realized without undue detriment to the patient’s quality of life.
Future Trends in Needle Biopsies and Other Non-Invasive Technologies
In recent times, many changes in the techniques and technology used for needle biopsies have brought promise of improved outcomes. Some examples include the use of coaxial or introducer needles that limit the area of disturbance of the malignant tissue, or cryoablation-guided techniques, where the surrounding tissue is frozen while the biopsy sample is being withdrawn (9). Less invasive options are also emerging, such as liquid biopsies, which detect cancer cells or DNA from a blood sample. These innovative approaches offer diagnostic insights without the invasive nature of traditional biopsies, reducing the associated risks and discomfort. As medical technology advances, the use of such non-invasive techniques is expected to increase, offering safer diagnostic alternatives and shaping the future of cancer care.
In addition to biopsies, modern imaging methods are providing in-depth information about cancer at the tissue level that was previously unavailable. For instance, combining MRI with spectroscopic analysis or quantitative transmission (QT) imaging yields a wealth of information, with the capability of pinpointing the location and nature of malignant tissues.
Hope4Cancer’s Approach to Biopsies and Whole-Body Health
Integrative oncology provides a holistic approach to cancer care that emphasizes the patient’s overall well-being and individual needs rather than focusing solely on the cancer. At Hope4Cancer Treatment Centers, we recognize that the decision to undergo a biopsy is deeply personal and varies depending on each patient’s unique situation. We support our patients regardless of their choice, understanding that some may opt for a biopsy while others might decline.
While most of our patients arrive with a pre-established diagnosis, in some cases, we do need to recommend some diagnostic measures. In the event that we do recommend a biopsy to a patient, we thoroughly explain the medical rationale for our recommendation and the associated risks versus benefits. In the end, we respect their wishes, whether they choose to go down that path or not. We also personalize the diagnostic approach used for each patient based on their specific needs by recommending other high–precision imaging methods, including MRIs and PET scans, while educating patients on how to mitigate some of the toxicities that may arise from radiation-based scans.
Our integrative approach is designed to support the body’s health comprehensively, whether a specific cancer diagnosis has been made through a biopsy or not. The therapies we offer are not limited to targeting one type of cancer but work synergistically to enhance the overall health of the body. This includes restoring the immune system’s function, enriching cells with oxygen, nutritionally supporting and detoxifying the body, and targeting cancer stem cells. In addition, even if a patient opts to have a biopsy, our therapies can be incredibly beneficial in helping to “mop up” potential issues such as seeding. Our holistic approach ensures that even if seeding occurs, the body is better prepared to address and manage these stray cells effectively.
Coming to Hope4Cancer offers patients an additional layer of comprehensive care, whether they choose conventional cancer treatments or not. Our supportive therapies are designed to maximize overall health and minimize the risks associated with traditional treatment and diagnostic methods, such as biopsies. By integrating these innovative and holistic approaches, Hope4Cancer ensures that each patient’s care plan is both thorough and tailored, making it a crucial component of effective cancer management and recovery.
References
1. Maseki, H., Jimbo, K., Watase, C. et al. Clinical significance of tumor cell seeding associated with needle biopsy in patients with breast cancer. Asian J Surg, 2023, 46: p. 3700-3704.
2. Yoneyama, K., Nakagawa, M., Hara, A. Local recurrence of breast cancer caused by core needle biopsy: Case report and review of the literature. Int J Surg Case Reports, 2020, 72: p. 318-321.
3. Harter, L.P., Curtis, J.S., Ponto, G. et al. Malignant seeding of the needle track during stereotaxic core needle breast biopsy. Radiology, 1992, 185: p. 713-714.
4. Ishizuna, K., Ota, D., Okamoto, J., et al. A case of mucinous carcinoma of the breast in which needle tract seeding was diagnosed by preoperative diagnostic imaging. Breast Cancer, 2011, 18: p. 324-327.
5. Szabo, B., Ojo, A., Al-Okati, D. MRI diagnosis of needle tract tumor seeding following core biopsy of mucinous carcinoma of the breast. Cureus, 2021, 13(4): e14493.
6. Chao, C., Torosian, M.H., Boraas, M.C. et al. Local recurrence of breast cancer in the stereotactic core needle biopsy site: Case reports and review of the the literature. The Breast J, 2002, 7(2): p. 124-127.
7. Nia, H.T., Munn, L.L., Jain, R.K. Physical traits of cancer. Science. 2020; 370 (6516): eaaz0868.
8. Stylianopoulos, T., Martin, J.D., Chauhan, V.P., et al. Causes, consequences, and remedies for growth-induced solid stress in murine and human tumors. Proc Natl Acad Sci USA 2012;109(38):p. 15101-8.
9. Holmes, D.R. Reducing the risk of needle tract seeding or tumor cell dissemination during needle biopsy procedures. Cancers, 2024, 16(2): 317.