Introduction
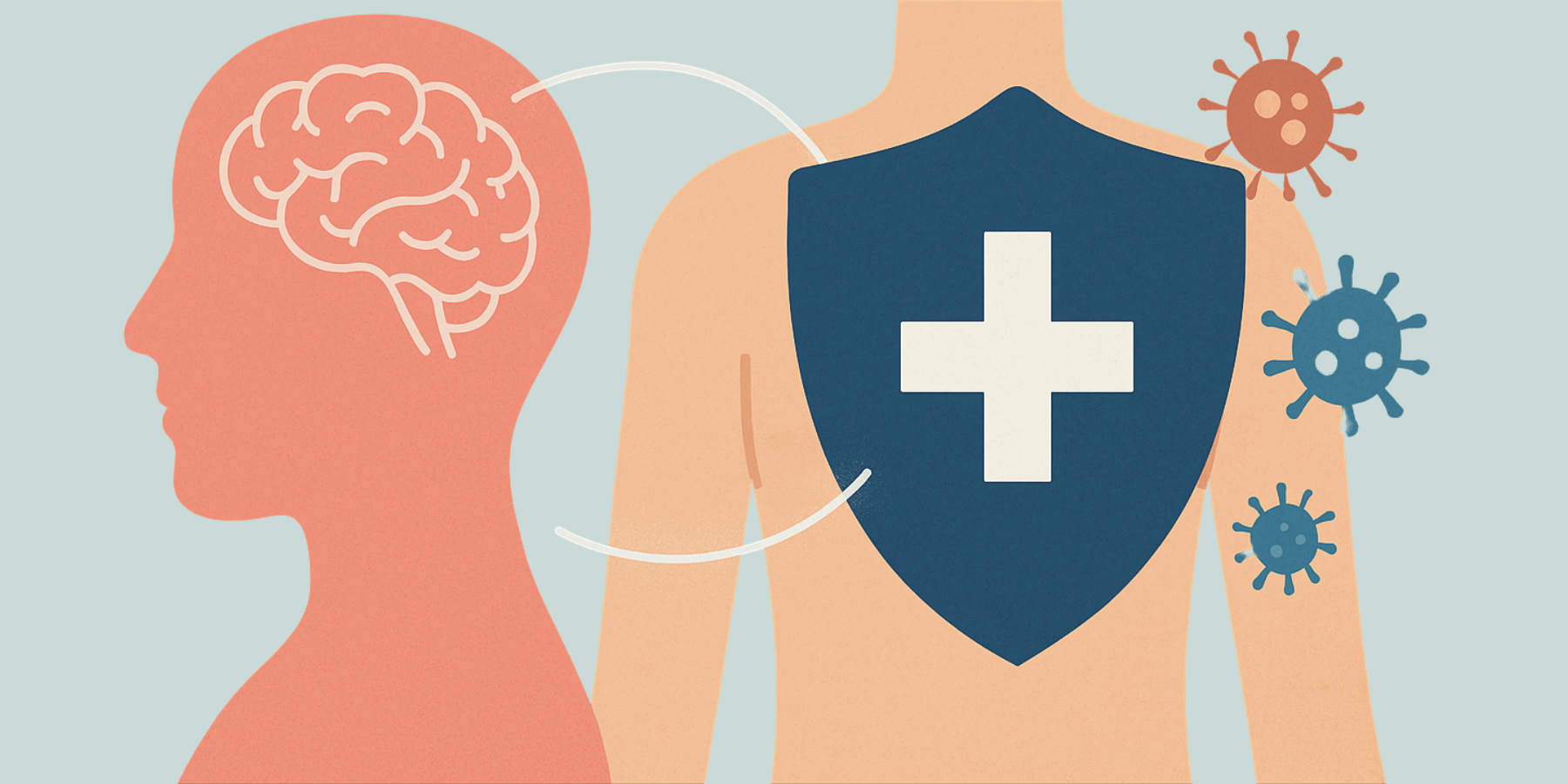
We’ve all felt it—the heavy fog of grief that seems to invite illness, or the electric buoyancy that follows a belly laugh. Emotions don’t just reside in the mind; they echo through the entire body, whispering—sometimes shouting—to our immune system.
Today, science is illuminating the depth of this mind-body dialogue. Chronic stress can unhinge immune balance, while joy may fortify it. At the same time, inflammation—the immune system’s internal alarm—can alter our emotional state, sometimes trapping us in feedback loops of fatigue, irritability, or sadness.
This is more than poetic intuition. Emerging research in psychoneuroimmunology is mapping the interface between the nervous, endocrine, and immune systems—revealing a dense network of biochemical signals, from hormones and cytokines to gut microbes and neuropeptides. In this article, we’ll explore how emotions and immunity shape each other—and why listening to this hidden conversation may be vital to our long-term health.
Emotions as Immune Conductors
Stress: A Double-Edged Sword
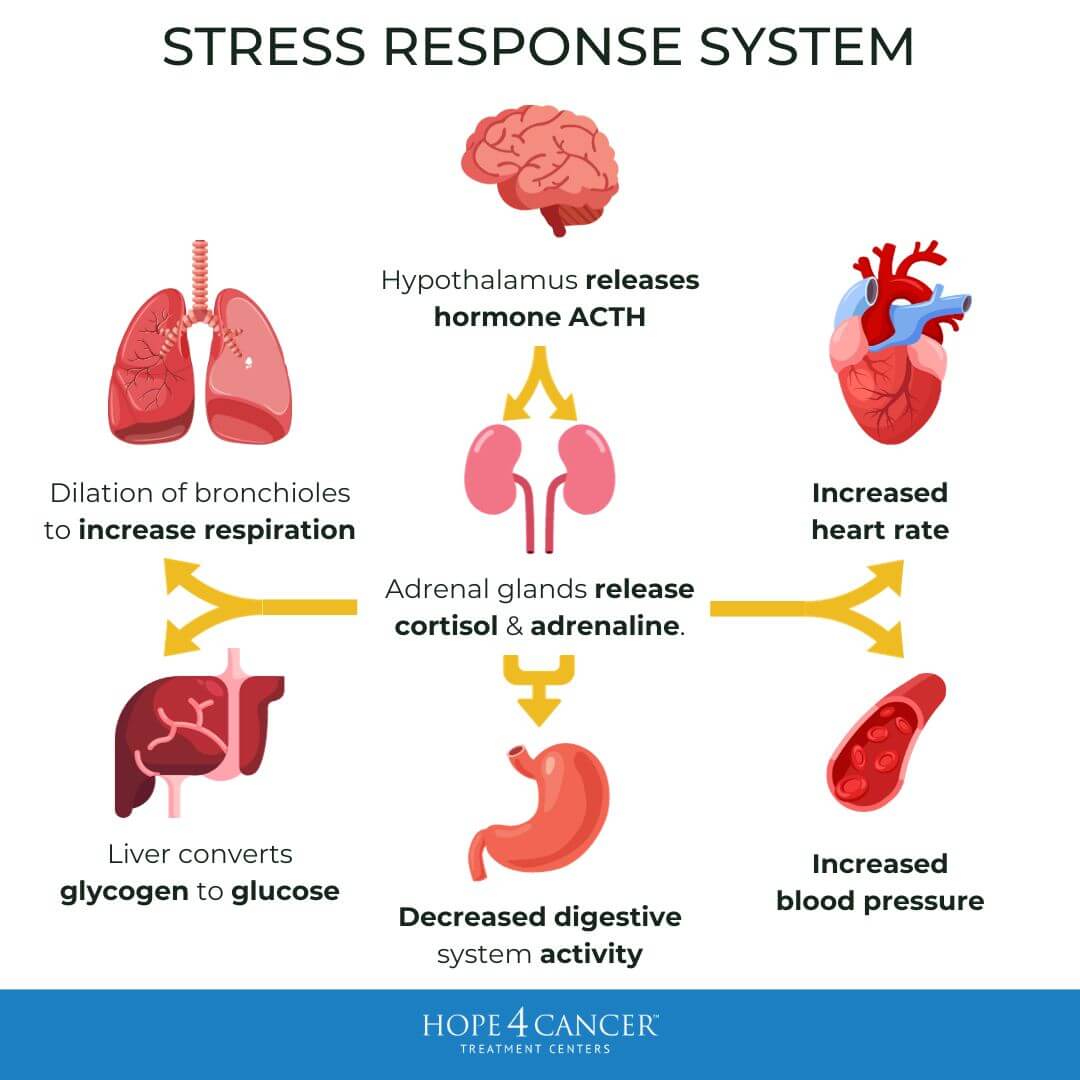
Stress isn’t always the villain. In brief doses—like when hitting an important deadline or escaping danger—it sharpens focus and mobilizes immune defenses. Studies show acute stress can enhance innate immunity by priming the inflammatory response (1-3) .
However, when stress becomes chronic, the story shifts. Initially, cortisol helps regulate inflammation, but long-term exposure leads to glucocorticoid resistance—which effectively results in immune cells becoming less sensitive to cortisol.
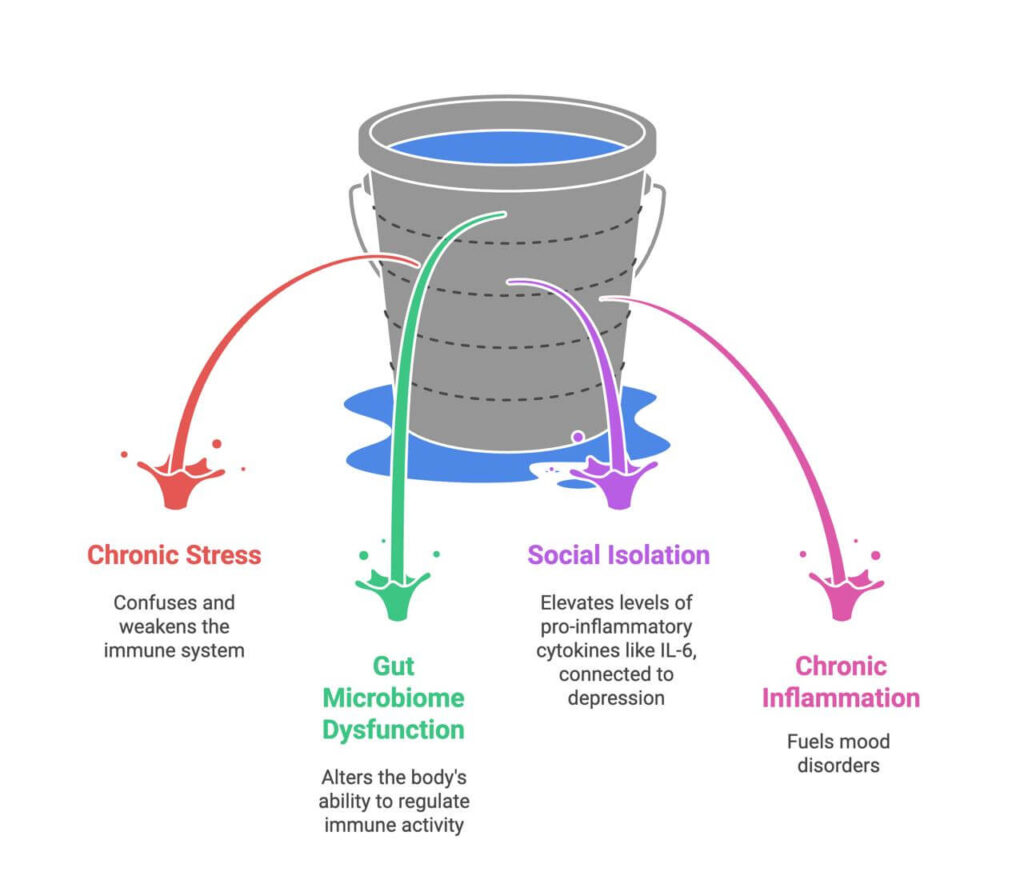
The result? A confused immune system—overactive in some ways, sluggish in others—linked to slower wound healing, more frequent colds, and weaker overall immune responses (4) .
The Gut Connection
Chronic stress also alters the gut microbiome, a key regulator of immune activity. In mice, stress- induced loss of protective microbial strains led to heightened inflammation—but probiotic supplementation reversed these effects (5) .
Loneliness: A Stealthy Immune Disruptor
Loneliness doesn’t just feel painful—it’s biologically potent. Perceived social isolation correlates with elevated levels of pro-inflammatory cytokines such as IL-6. In prehistoric times, isolation may have triggered heightened immune vigilance which was needed for survival, but in modern life this contributes to chronic disease risk, depression, cardiovascular problems, and even accelerated aging (6) .
Joy, Laughter, and Immune Strength
On the brighter end of the spectrum, positive emotions strongly modulate immunity. Those with high emotional well-being show stronger antiviral gene expression—especially Type I interferon-related responses (7) . And laughter? It boosts natural killer (NK) cell activity, supporting immune surveillance against infections and even cancer (8) .
The Immune System Talks Back: How Inflammation Shapes Mood
Cytokines: Messengers of Mood
When inflammation is high, immune mediators like IL-1, IL-6, and TNF-α signal the brain—triggering “sickness behavior”: fatigue, reduced appetite, social withdrawal, all to promote rest and recovery. But when inflammation becomes chronic, it can fuel sustained mood disorders.
Around 30% of people with depression show elevated inflammatory markers. Recent trials targeting IL-6 have reduced depressive symptoms, particularly in those with high baseline inflammation (9) . Chronic inflammation can also disrupt neurotransmission—TNF-α interferes with dopamine and serotonin pathways, contributing to “brain fog” (10) .
The Microbiome’s Mood-Modulating Role
The gut microbiota produce dozens of neuroactive compounds—including 90% of the body’s serotonin. In a landmark study, rodents receiving microbiota transplants from depressed humans began exhibiting depressive behavior (11) —underscoring how literally emotional health begins in the gut.
Breaking the Cycle: Practical Ways to Harmonize Mood and Immunity
The feedback loop between mood and immunity is dynamic—and modifiable. Here are evidence-based strategies:
- Move with Moderation: Exercise reduces inflammation, boosts levels of the critical brain-derived neurotrophic factor (BDNF) protein, and lifts mood. But balance is key—overtraining can elevate cortisol and suppress immunity (12).
- Integrate Muscle-Based Biochemistry: It’s not just about perception—our movement sends direct physiological messages. When muscles contract, they release myokines, such as IL-6, which differ from immune-derived IL-6. Exercise-induced IL-6 has anti- inflammatory effects, enhances glucose metabolism, and prompts a controlled cortisol response—making movement not just training, but therapeutic (13).
- Nurture Social Bonds: Connection, even virtually or through small acts of kindness, can lower inflammatory gene expression (14) .
- Feed Your Microbes: Diets rich in polyphenols (berries, greens, turmeric) and fermented foods (kefir, sauerkraut, kimchi) support gut diversity—linked to reduced anxiety and stronger immune function.
- Practice Mindfulness (Not Perfection): Short daily practice—10 minutes—can dampen NF-κB activation, a key driver of inflammation (15).
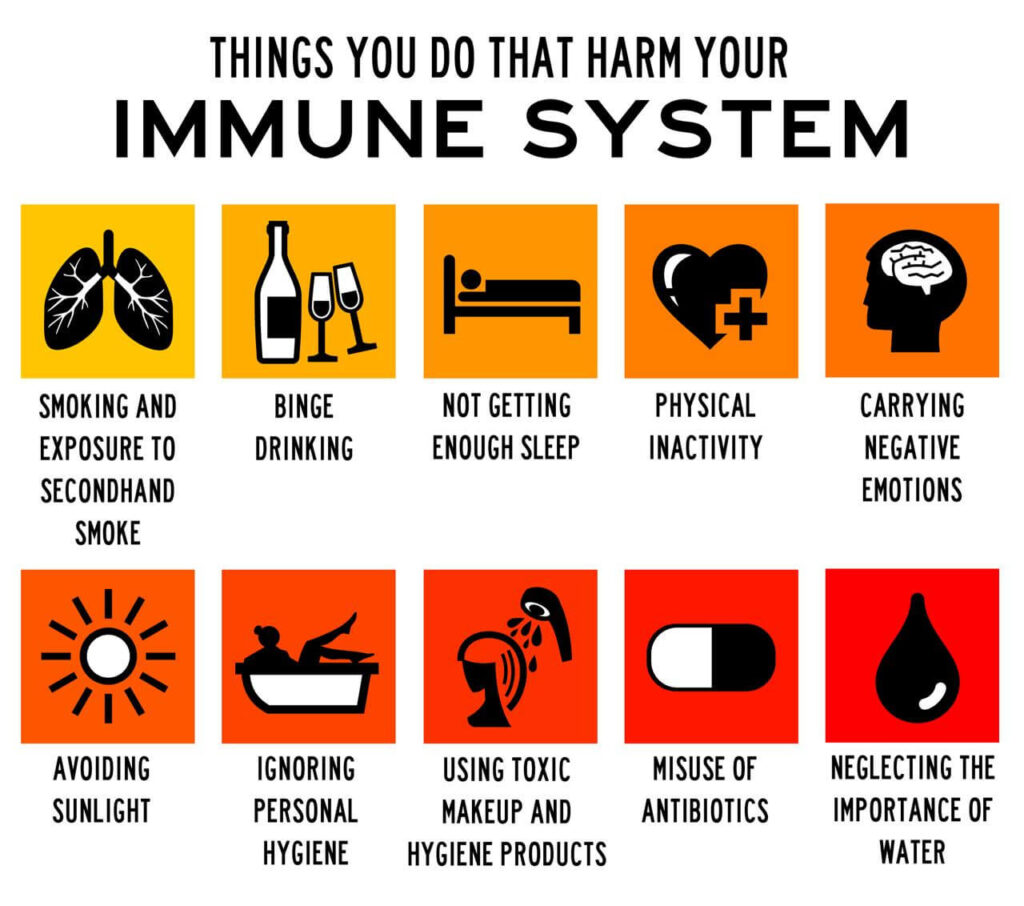
While this article has focused on the powerful connection between emotions and immune function, it’s important to remember that immunity is also shaped by the physical choices we make every day. Lifestyle factors such as sleep, movement, nutrition, and hygiene create the foundation on which our emotional–immune balance rests. The infographic below highlights some common habits—both emotional and physical—that can quietly erode immune resilience over time.
Conclusion
Emotions and immunity are interwoven strands in the same biological tapestry. Joy can bolster immune defenses; persistent worry can unravel them. Likewise, an overactive immune system can reshape our emotional landscape.
But within this dance lies powerful opportunity. By caring for our emotional health, we enhance immune resilience. And by nurturing our physical well-being—via sleep, connection, movement, and nourishment—we uplift the emotional states that bring life meaning.
As Hippocrates reminded us, “Healing is a matter of time, but it is sometimes also a matter of opportunity.” Today, that opportunity lies in listening to the subtle dialogue between our thoughts, our cells, and our immunity—and learning how to respond with care.
References:
- Dhabhar FS. Effects of stress on immune function: the good, the bad, and the beautiful. Immunol Res 2014, 58:193–210.
- Dhabhar FS. Enhancing versus suppressive effects of stress on immune function: implications for immunoprotection and immunopathology. Neuroimmunomodulation 2009, 16:300–17.
- Dhabhar FS, Saul AN, Daugherty C, et al. Short-term stress enhances cellular immunity and increases early resistance to squamous cell carcinoma. Brain Behav Immun 2010, 24:127–37.
- Cohen S, Tyrrell DA, Smith AP. Psychological stress and susceptibility to the common cold. N Engl J Med 1991, 325:606–12.
- Ritz NL, Draper LA, Bastiaanssen TFS, et al. The gut virome is associated with stress- induced changes in behaviour and immune responses in mice. Nat Microbiol 2024, 9:359–76.
- Van Bogart K, Engeland CG, Sliwinski MJ, et al. The Association Between Loneliness and Inflammation: Findings From an Older Adult Sample. Front Behav Neurosci 2021, 15:801746.
- Cole SW, Cacioppo JT, Cacioppo S, et al. The Type I interferon antiviral gene program is impaired by lockdown and preserved by caregiving. Proc Natl Acad Sci U S A 2021, 118.
- Bennett MP, Zeller JM, Rosenberg L, et al. The effect of mirthful laughter on stress and natural killer cell activity. Altern Ther Health Med 2003, 9:38–45.
- Ting EY, Yang AC, Tsai SJ. Role of Interleukin-6 in Depressive Disorder. Int J Mol Sci 2020, 21.
- Felger JC, Li Z, Haroon E, et al. Inflammation is associated with decreased functional connectivity within corticostriatal reward circuitry in depression. Mol Psychiatry 2016, 21:1358–65.
- Kelly JR, Borre Y, C OB, et al. Transferring the blues: Depression-associated gut microbiota induces neurobehavioural changes in the rat. J Psychiatr Res 2016, 82:109–18.
- Gleeson M, Bishop NC, Stensel DJ, et al. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol 2011, 11:607–15.
- Pedersen BK, Febbraio MA. Muscle as an endocrine organ: focus on muscle-derived interleukin-6. Physiol Rev 2008, 88:1379–406.
- Black DS, Slavich GM. Mindfulness meditation and the immune system: a systematic review of randomized controlled trials. Ann N Y Acad Sci 2016, 1373:13–24.
- Dutcher JM, Cole SW, Williams AC, et al. Smartphone mindfulness meditation training reduces Pro-inflammatory gene expression in stressed adults: A randomized controlled trial. Brain Behav Immun 2022, 103:171–7.